How progress within cardiac devices is changing priorities for physiologists
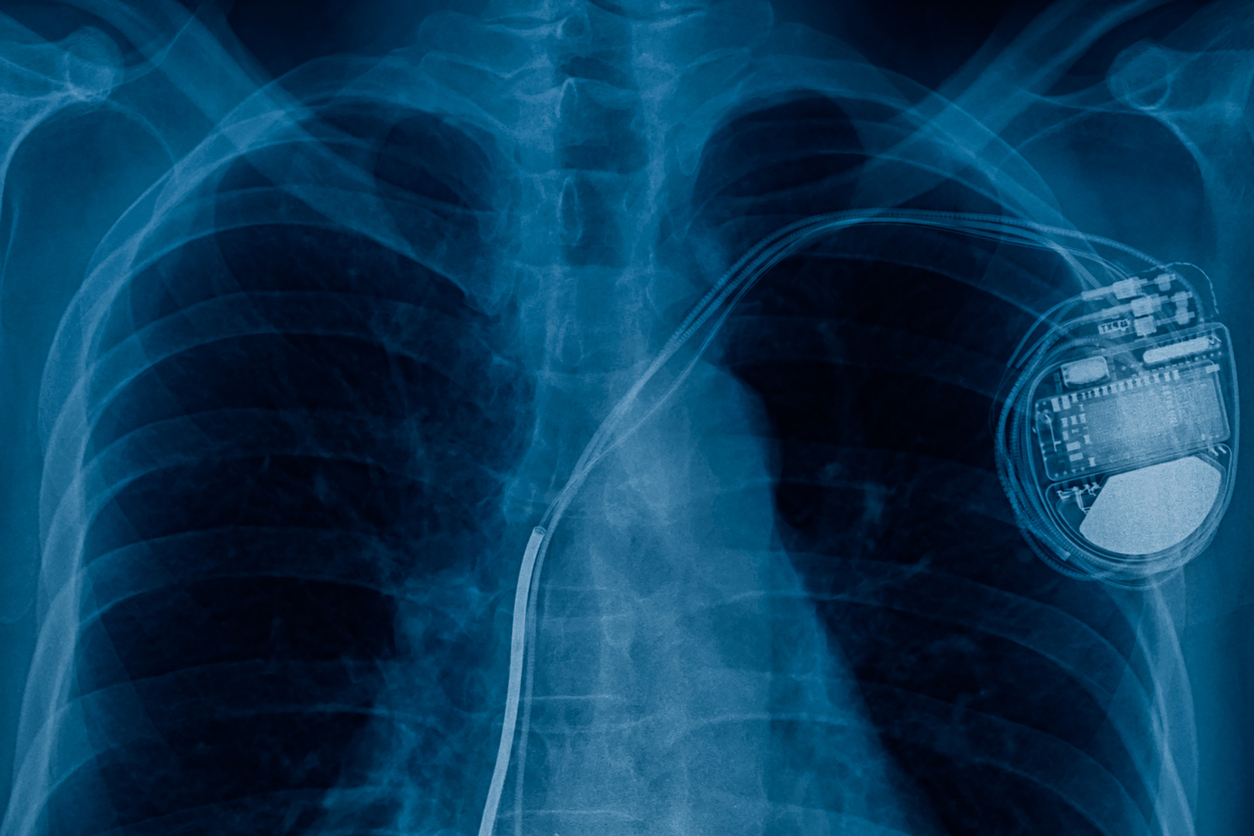
The development of technology has greatly enhanced the capabilities of pacemakers and implantable cardiac defibrillators (ICDs) which now have the ability to provide more data about a patient’s health than ever before. Cardiac Physiologists now have a window on the overall health of their patients, in addition to the ‘health’ of the implanted device. PACENET’s Advisor and Principal Cardiac Physiologist at Imperial College Healthcare NHS Trust, Ian Wright, speaks to PACENET about how the progress that is being made within medical devices is changing the priorities for physiologists.
What is a pacemaker or ICD for?
A pacemaker or ICD is implanted for a particular indication, for a specific condition. This intervention may be required for a variety of different reasons, from preventing a patient from experiencing blackouts due to a slow heart rhythm, to protecting an individual from facing a potential cardiac arrest in the future.
Our principal goal as physiologists will always be to ensure implanted devices operate effectively and efficiently. However, with progress in technology, pacemakers and ICDs have become increasingly intelligent; to the point where they now have the capacity to deliver powerful data about a patient’s health – offering new options for clinical management. For example, a device that has the ability to record signals from the atrium can automatically alert us when a patient develops atrial fibrillation, which could lead to a stroke if not treated with anticoagulants. This intelligence increasingly means that the utility of these devices can be stretched beyond their primary purpose.
New potential
Cardiac devices can now contribute to the diagnosis of new conditions, enabling appropriate treatment to be initiated. Sophisticated sensors can detect a suite of physiological markers that may suggest that a patient is rapidly deteriorating from heart failure – this equips us with the knowledge to intervene and provides crucial time to potentially save a life. This approach, where device detection is followed by clinical intervention, requires an expansion of the original objectives of device therapy – challenging physiologists to broaden our scope and expand how we can treat our patients.

By adding new skills of clinical management on top of a firm technical foundation, we have the opportunity to improve the management of long-term chronic conditions such as heart failure. In the future, patients with conditions such as frailty and dementia could potentially benefit from data derived from their device. Using this information, the device follow-up department could then equip patients with the earliest and most appropriate treatments to prevent a decline in health.
We are currently only scratching the surface of the potential capabilities of implanted cardiac devices. For example, let’s take the mobile phone. You have to explain to teenagers nowadays that once upon a time the purpose of a mobile phone was to call someone! Now in 2021, for many people, ringing someone is almost a forgotten feature; the device has been transformed into a tool for browsing the internet, posting on social media and catching up on your favourite Netflix series. These applications have been built on top of the original foundation. For cardiac devices, new layers of additional functionality are being built on top of the primary function of electrically stimulating the heart.
Infrastructure and systems
For the mobile to become the smartphone required a critical number of users, developers to build attractive apps, and the infrastructure and communications systems put in place to allow fast data transmission. The increased popularity of smartphones was critically dependent on the establishment of a backbone of 4G infrastructure. In the same way, the elements necessary for realising the great potential offered by device data are being put in place. The technology behind remote-monitoring has become increasingly sophisticated and user-friendly, and the emergence of the Covid-19 pandemic, and the resulting directives for the public to stay at home, has driven a tremendous acceleration in the number of patients connecting their devices via home-monitoring.
As a result, we now have the building blocks in place for significant innovation in the use of remotely monitored cardiac device data. But it will still require imagination and creativity to fully realise the potential of the technology. To really improve patient health, we will have to adopt new ways of thinking, new processes and new systems. We will need to work differently to apply the technology in the most innovative ways. We need to ask the question: how can we use remote monitoring to better interact with our patients and improve their health? The ability to identify patients who are declining due to heart failure is a significant leap. But once we have the right mind-set, the right systems and the right infrastructure in place we can utilise this knowledge about the patient to actually change the outcome, to prevent the need for hospital admission, or in some instances, to prevent the death of a patient. That is revolutionary.
So, we are now in possession of a well-developed technology for remote-monitoring which is becoming more universal and which makes it possible to evaluate patients from the comfort of their own homes. Making data more accessible is a key step in this evolution. We are used to PACENET enabling us to quickly, efficiently and confidently locate every patient with a device or lead that is the subject of a medical device alert. But having information made simple, readily accessible and accurate through PACENET also means that, as clinicians, we are equipped with the information we need to make informed decisions based on clinical risk. PACENET provides a hub for all the information from the implanted device to come together with technical and clinical history in one place; saving time and allowing for effective clinical evaluation.

Integration and Collaboration
Physiologists usually do not have the power to refer patients directly. Device follow-up units also lack the integration with other departments and other specialities needed to be able to direct patients onwards onto the right pathway to receive optimal treatment. Integration with community services and general practice is limited or completely absent. Often the only option is to admit a patient to hospital, when it may be better for them to be treated in their own home. There needs to be a better level of integration and greater autonomy in order to enable physiologists to coordinate patient care and guide them through a particular treatment pathway. With an increasing number of patients using remote-monitoring systems, increased collaboration and shared decision-making with a far greater range of clinicians and other healthcare professionals will be critical. This level of partnership is a challenge as it requires effective interpersonal communication and integration across IT systems.
Conclusion
Progress made within implanted cardiac devices over recent years has been nothing short of extraordinary. But we need to continuously push the boundaries of innovation. Working in isolation can only take us so far. In order to achieve even more with implanted cardiac devices, we need to bring together different perspectives, contrasting points of view; and stretch ourselves. Collaboration and information need to be at the heart of everything we do.
– Ian Wright, PACENET’s Advisor and Principal Cardiac Physiologist at Imperial College Healthcare NHS Trust